Is there a link between poverty, crowded accommodation, and Africa’s bafflingly low infection and death rates from the pandemic?
As the number of infections dips sharply in South Africa, and stays relatively low across much of the continent, experts are reaching towards a startling hypothesis.
Crowded townships. Poor hygiene. The impossibility of social distancing in communities, where large families often share a single room.
For months health experts have been warning that living conditions in poor, urban communities across Africa are likely to contribute to a rapid spread of coronavirus.
“Population density is such a key factor. If you don’t have the ability to social distance, the virus spreads,” said Professor Salim Abdool Karim, the head of South Africa’s ministerial advisory team on Covid-19.

But what if the opposite is also true?

What if those same crowded conditions also offer a possible solution to the mystery that has been perplexing experts on the continent for months?
What if – and this is putting it rather crudely – poverty proves to be the best defence against Covid-19?
MORE:
‘It’s an enigma’
Let’s start with that mystery. In the early stages of the pandemic, all the experts and all the modelling agreed that Africa was in trouble.
“I thought we were heading towards a disaster, a complete meltdown,” said Professor Shabir Madhi, South Africa’s top virologist.
Even the most optimistic predictions showed that the nation’s hospitals – and the continent’s most developed health system – would be quickly overwhelmed.
And yet, today South Africa is emerging from its first wave of infections with a Covid-19 death rate roughly seven times lower than the UK’s.
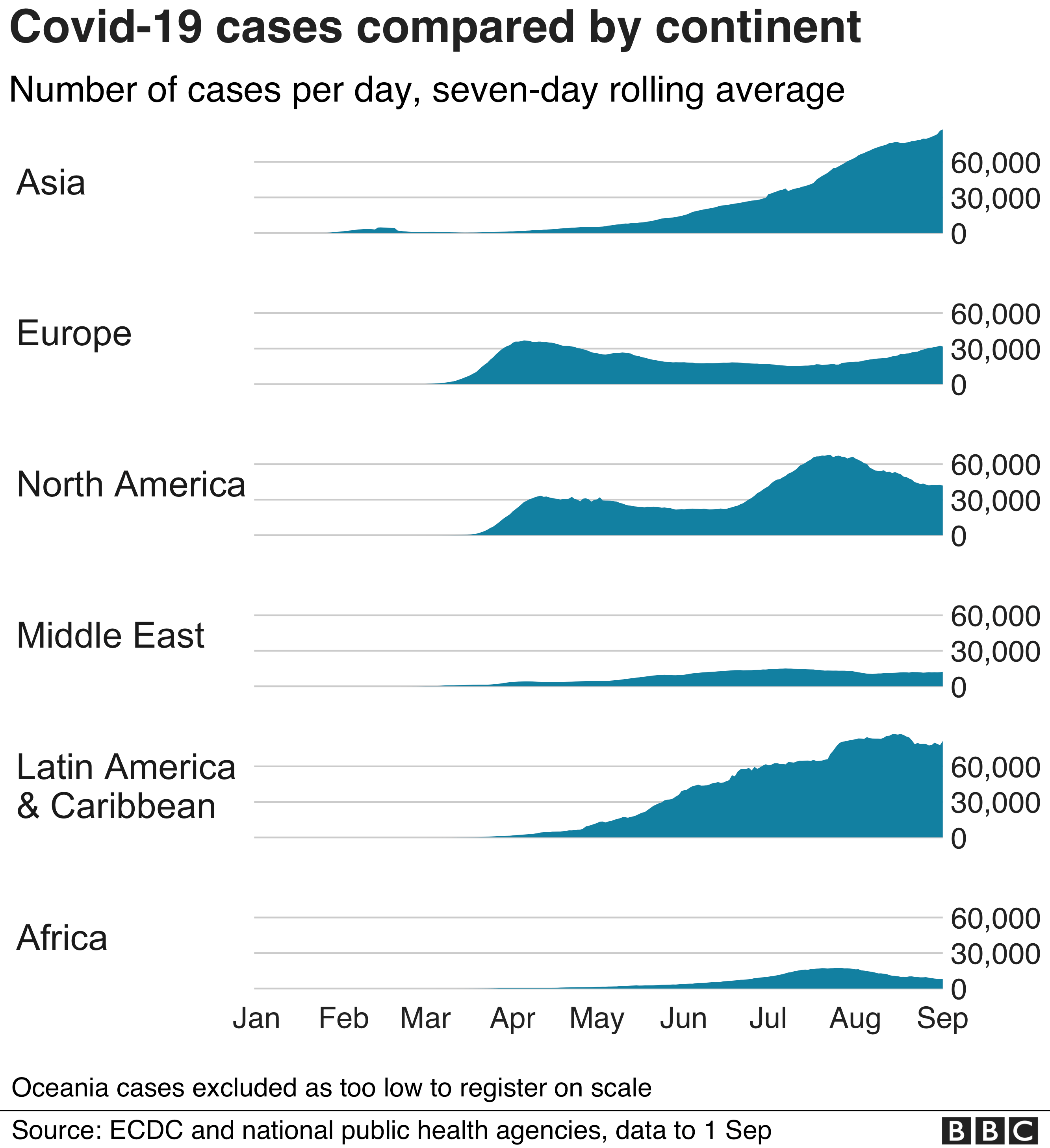

Even if deaths have been under-reported here – perhaps by a factor of two – South Africa has still performed impressively well, as have many other parts of the continent, where hospital beds remain stubbornly empty, and where infection graphs have almost entirely avoided the pronounced peaks and sharp angles seen in so many other parts of the world.
“Most African countries don’t have a peak. I don’t understand why. I’m completely at sea,” admitted Prof Karim, a leading voice on South Africa’s pandemic response.
Professor Madhi agrees: “This is an enigma. It’s completely unbelievable.”
For a while now, experts have cited a youthful population as the best explanation for Africa’s relatively low infection rates.
After all, the average age on the continent is roughly half that in Europe.
Far fewer Africans live into their 80s, and so are less likely to succumb to the virus as a result.
“Age is the highest risk factor. Africa’s young population protects it,” said Tim Bromfield, a regional director of the Tony Blair Institute for Global Change.
But as the pandemic drags on, and the statistical evidence builds up, analysts appear increasingly reluctant to give demographics all the credit for this continent’s successes.”
Age is not such a big factor,” said Prof Karim.Early, and aggressive lockdowns here in South Africa and elsewhere on the continent have clearly played a crucial role.
Clear messaging about masks and the provision of oxygen supplies have also been important.
Other theories – about the impact of altitude or warmer temperatures – have generally been pushed aside.Some experts warn that a vast and poorly connected continent may simply be biding its time, and that the virus could strike hard in the coming months.
“I would not venture to say that Africa is over its worst. I’m not sure whether one day the epidemic is going to spread like crazy here,” said Prof Karim.
Other coronaviruses
But in recent days, scientists at the Vaccine and Infectious Disease Analytics unit, at Baragwanath hospital in Soweto, have been wondering if the missing factor – the answer to what they see as the continent’s pandemic mystery – might lie inside a glorified chest freezer in their laboratory, on the outskirts of Johannesburg.
The freezer, whose temperature is kept at minus 180C, thanks to liquid nitrogen – contains metal cannisters storing five-year-old human blood samples.
Or to be more specific, extracts from blood cells – known as PBMCs – acquired during an earlier influenza vaccine trial in Soweto.
![Quote card. Professor Shabir Madhi: "The protection might be much more intense in highly populated areas, in African settings. It might explain why the majority [on the continent] have asymptomatic or mild infections"](https://c.files.bbci.co.uk/4DDB/production/_114213991_582e7b78-fee5-45f6-b228-e649c598eff5.png)
The idea is that, by studying the PBMCs, the scientists might find evidence that people had been widely infected by other coronaviruses – those, for instance, responsible for many common colds – and that, as a result, they might enjoy some degree of immunity to Covid-19.
“It’s a hypothesis. Some level of pre-existing cross-protective immunity… might explain why the epidemic didn’t unfold [the way it did in other parts of the world],” said Prof Madhi, explaining that data from scientists in the US appeared to support the hypothesis.
Colds and flu are, of course, commonplace around the world.
But the South African scientists wondered whether, because those viruses spread more effectively in overcrowded neighbourhoods, poorer communities might have been more widely exposed and therefore, enjoy a larger degree of immunity towards Covid-19.
The same, of course, could apply to other parts of the world, like India, with similar challenges.
“The protection might be much more intense in highly populated areas, in African settings. It might explain why the majority [on the continent] have asymptomatic or mild infections,” said Prof Madhi.
“I can’t think of anything else that would explain the numbers of completely asymptomatic people we’re seeing. The numbers are completely unbelievable,” he said, savouring the irony of the possibility that Africa’s entrenched poverty might “for once” work in the continent’s favour.
Sceptics though might point to countries like Brazil, with its crowded favelas, and its high infection rate.

Unfortunately, as the scientists began preparing to test the PBMC samples in their laboratory, they spotted a problem.
A quality-control test revealed that the icy temperature inside the cryo-containers had fluctuated over time – too much for the rigorous standards required for such an important and delicate experiment.
“We’re very disappointed. We were all ready but unfortunately this thing happened,” said Doctor Gaurav Kwatra, who was leading the experiment.
There was no-one to blame – not even South Africa’s notorious power-cuts. It was just one of those things.
The team is now busy hunting for new samples to test, but that may take months.
In the meantime, the mystery of Africa’s relatively mild pandemic lives on.

