Nigeria has announced that free emergency Caesarean sections will be made available to “poor and vulnerable”women in an ambitious plan to bring down the high number of mothers dying in childbirth.
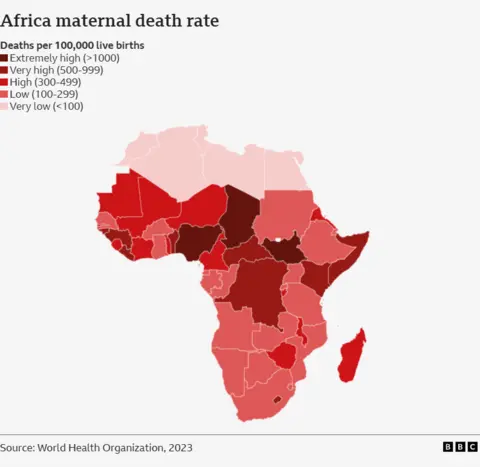
At 1,047 deaths per 100,000 live births, Africa’s most populous nation has the fourth-highest maternal mortality rate in the world and the lack of access to Caesareans is thought to be one of the reasons.
Many pregnant women, particularly in rural Nigeria are unable to receive emergency medical care partly due to the cost.
“No woman should lose her life simply because she can’t afford a C-section,” Health Minister Muhammad Pate said while announcing the “powerful move”.
While the price may vary across Nigeria’s different states, on average, a Caesarean costs around 60,000 naira ($36; £28) – which can be beyond the reach of many.
More than 40% of Nigerians live below the international extreme poverty line of $2.15 per day, according to 2023 data from Nigeria’s National Bureau of Statistics.
The Maternal Mortality Reduction Innovation Initiative launched on Thursday will now allow all eligible women to access Caesarean sections in public hospitals.
To be a beneficiary, one must be registered under the country’s public health insurance scheme.
“By removing financial barriers to this life-saving procedure, we ensure that no woman in need is denied critical care due to cost,” Pate added.
The health scheme covers emergencies only, Tashikalmah Hallah, a communication adviser to the health minister, told the BBC.
Social welfare units in public hospitals would help determine eligibility and identify those who can not afford the procedure, Mr Hallah added.
Pate said maternal mortality remained “unacceptably high”.
Caesareans are seen as essential for preventing obstructed labour in cases where a woman’s pelvis is too small, the baby is in a breech position or is too large to exit the birth canal.
Without intervention, a constricted baby may fatally rupture the uterus, or cause tears that catastrophically haemorrhage.
While offering to support the new initiative, the World Bank’s Trina Haque, described it as a “game-changer”.
“If implemented right, this initiative will deliver. We’re here to support every step of the way,” Kazadi Mulombo, the UN World Health Organization (WHO) country representative, said.
Causes of maternal deaths include severe haemorrhage, high blood pressure (pre-eclampsia and eclampsia), unsafe abortions and obstructed or prolonged labour.
The new policy would “improve maternal and child health outcomes in the country”, said Rhoda Robinson, executive director of HACEY, a non-governmental organisation (NGO) advocating for healthcare access for vulnerable populations in Nigeria.
“Especially for women from low-income communities who might resort to alternative and often unsafe care options,” she told the BBC.
Mabel Onwuemena, national coordinator of the Women of Purpose Foundation, another NGO advocating for better maternal health access in Africa, praised the initiative and urged the Nigerian government to expand it to include free drugs and ultrasound for pregnant women.
ALSO READ:

